We interviewed Suzanne Goh MD about mitochondrial dysfunction, which is common in children with seizures and neurodevelopmental disorders such as autism.
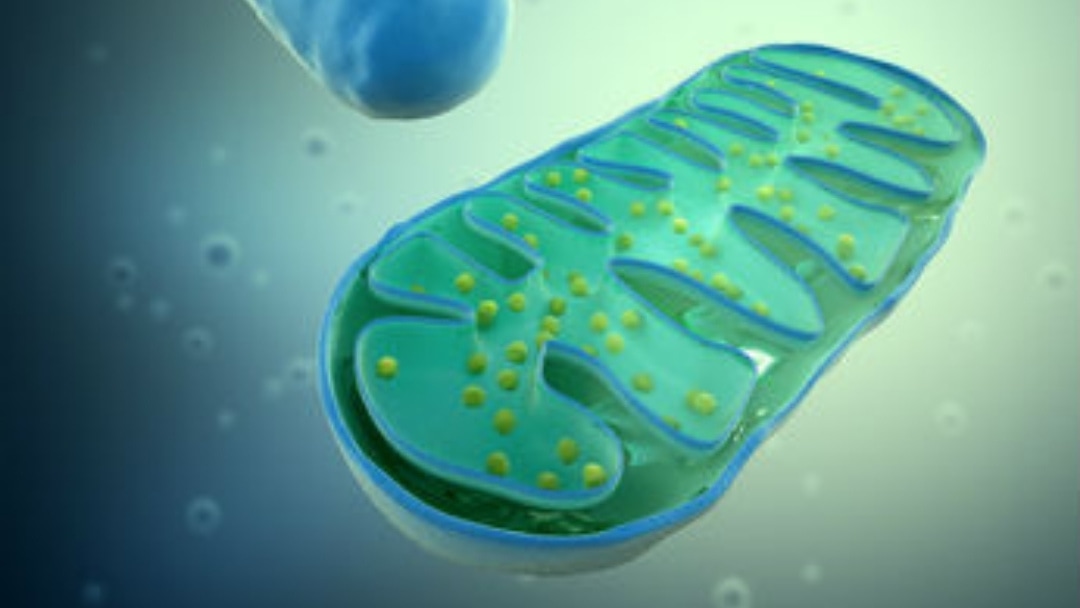
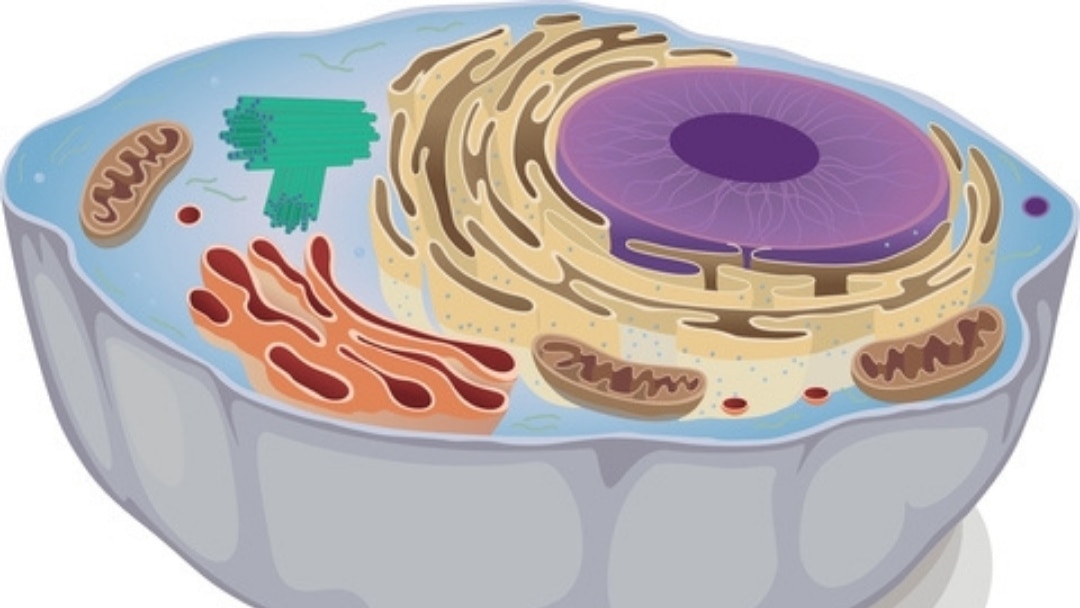
The best way to think of mitochondrial dysfunction is like thinking about economics: supply and demand. People with mitochondrial dysfunctions can’t supply enough energy to meet their bodies’ demands. Seemingly typical things to most people can cause an energy drain in those with mitochondrial dysfunction.
Breakthroughs in neurological research have shown the essential role of mitochondria to healthy brain function and development. Key nutrients to target mitochondrial function can have a positive impact on language, communication, and social ability – from infancy to adulthood.
Watch this webinar to find out more about this subject that might be more common than is currently suspected.
Please note that you will be asked to enter your email address at the 30-minute mark to finish viewing the video.
About Suzanne Goh MD
 Dr. Suzanne Goh is a board-certified pediatric behavioral neurologist, a neuroscience researcher, and author. She has dedicated her career to researching and developing therapies for neurological conditions that impact childhood brain development.
Dr. Suzanne Goh is a board-certified pediatric behavioral neurologist, a neuroscience researcher, and author. She has dedicated her career to researching and developing therapies for neurological conditions that impact childhood brain development.
Specializing in the treatment of autism, she is the founder of Cortica, and creator of the Cortica Care Model.
Dr. Goh was born and raised in Toledo, Ohio. She pursued her undergraduate studies at Harvard University where she received her Bachelors of Arts degree, summa cum laude, in History and Science (1993-1997). She went on to attend Oxford University as a Rhodes Scholar (1997-1999). In 2004, she graduated from Harvard Medical School, cum laude.
Dr. Goh completed her Pediatrics Internship at Massachusetts General Hospital and her Pediatric Neurology Residency at University of California San Francisco.
You can find out more about her work at her website www.corticacare.com
Disclaimer
This webinar is not a substitute for medical advice, treatment, diagnosis, or consultation with a medical professional. It is intended for general informational purposes only and should not be relied on to make determinations related to treatment of a medical condition. Epidemic Answers has not verified and does not guaranty the accuracy of the information provided in this webinar.
Still Looking for Answers?
Visit the Epidemic Answers Practitioner Directory to find a practitioner near you.
Join us inside our online membership community for parents, Healing Together, where you’ll find even more healing resources, expert guidance, and a community to support you every step of your child’s healing journey.
Sources & References
Andreazza, A.C., et al. Mitochondrial complex I activity and oxidative damage to mitochondrial proteins in the prefrontal cortex of patients with bipolar disorder. Arch Gen Psychiatry. 2010 Apr;67(4):360-8.
Balcells, Cristy. Autism & Mitochondrial Disorders: How Much Do We Really Know?. MitoAction.org. 29 Jan 2009
Beal, M.F., et al. Therapeutic approaches to mitochondrial dysfunction in Parkinson’s disease. Parkinsonism Relat Disord. 2009 Dec;15 Suppl 3:S189-94.
Bradford, B.L., et al. Mitochondrial Dysfunction and Type 2 Diabetes. Science. 2005 Jan 21;307(5708):384-7.
Bradstreet, J.J., et al. Biomarker-guided interventions of clinically relevant conditions associated with autism spectrum disorders and attention deficit hyperactivity disorder. Altern Med Rev. 2010 Apr;15(1):15-32.
Burchell, V.S., et al. Targeting mitochondrial dysfunction in neurodegenerative disease: Part I. Expert Opin Ther Targets. 2010 Apr;14(4):369-85.
Burchell, V.S., et al. Targeting mitochondrial dysfunction in neurodegenerative disease: Part II. Expert Opin Ther Targets. 2010 May;14(5):497-511.
Davi, Alyssa. Has Your Child with Autistic Symptoms Been Properly Screened for a Subset of Mitochondrial Disease Known as OXPHOS?…Probably Not. Autism File. 2010; 36.
Dehley, Leanna M., et al. The Effect of Mitochondrial Supplements on Mitochondrial Activity in Children with Autism Spectrum Disorder. J Clin Med. 2017 Feb; 6(2): 18.
Ferrer, et al. Early involvement of the cerebral cortex in Parkinson’s disease: convergence of multiple metabolic defects. Prog Neurobiol. 2009 Jun;88(2):89-103.
Filipek, P.A., et al. Relative carnitine deficiency in autism. J Autism Dev Disord. 2004 Dec;34(6):615-23.
Haas, R.H., et al. Mitochondrial disease: a practical approach for primary care physicians. Pediatrics. 2007 Dec;120(6):1326-33.
Hao, J., et al. Mitochondrial nutrients improve immune dysfunction in the type 2 diabetic Goto-Kakizaki rats. J Cell Mol Med. 2009 Apr;13(4):701-11.
Herbert, M.R. Contributions of the environment and environmentally vulnerable physiology to autism spectrum disorders. Curr Opin Neurol. 2010 Apr;23(2):103-10
James, S.J., et al. Cellular and mitochondrial glutathione redox imbalance in lymphoblastoid cells derived from children with autism. FASEB J. 2009 Aug;23(8):2374-83.
Kato, T. The role of mitochondrial dysfunction in bipolar disorder. Drug News Perspect. 2006 Dec;19(10):597-602.
Kelley, R.I. Evaluation and Treatment of Patients with Autism and Mitochondrial Disease. Kennedy Krieger Institute, Division of Metabolism.
Klehm, M., et al. Clinician’s Guide to the Management of Mitochondrial Disease: A Manual for Primary Care Providers. MitiAction.org. 2014.
Konradi, C., et al. Molecular evidence for mitochondrial dysfunction in bipolar disorder. Arch Gen Psychiatry. 2004 Mar;61(3):300-8.
Korson, M. Mitochondrial Disease and Patient Challenges. MitoAction. 2008.
Leib, S., et al. Mitochondrial Oxidative Phosphorylation (OXPHOS) Dysfunction: A Newly Emerging Category of Autistic Spectrum Disorder Information for Primary Care Physicians. MitoAction.org. 2010.
Liu, J. The effects and mechanisms of mitochondrial nutrient alpha-lipoic acid on improving age-associated mitochondrial and cognitive dysfunction: an overview. Neurochem Res. 2008 Jan;33(1):194-203.
Long, J., et al. Mitochondrial decay in the of old rats: ameliorating effect of alpha-lipoic acid and acetyl-L-carnitine. Neurochem Res. 2009 Apr;34(4):755-63.
Mabalirajan, U., et al. Effects of vitamin E on mitochondrial and asthma features in an experimental allergic murine model. J Appl Physiol. 2009 Oct;107(4):1285-92.
Maes, M., et al. Coenzyme Q10 deficiency in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is related to fatigue, autonomic and neurocognitive symptoms and is another risk factor explaining the early mortality in ME/CFS due to cardiovascular disorder. Neuro Endocrinol Lett. 2009;30(4):470-6.
Maes, M., et al. Lower plasma Coenzyme Q10 in depression: a marker for treatment resistance and chronic fatigue in depression and a risk factor to cardiovascular disorder in that illness. Neuro Endocrinol Lett. 2009;30(4):462-9.
Morino, K., et al. Molecular mechanisms of insulin resistance in humans and their potential links with mitochondrial dysfunction. Diabetes. 2006 Dec;55 Suppl 2:S9-S15.
Noland, R.C., et al. Carnitine insufficiency caused by aging and overnutrition compromises mitochondrial performance and metabolic control. J Biol Chem. 2009 Aug 21;284(34):22840-52.
Oliveira, G., et al. Mitochondrial dysfunction in autism spectrum disorders: a population-based study. Dev Med Child Neurol. 2005 Mar;47(3):185-9.
Palmieri, L., et al. Mitochondrial dysfunction in autism spectrum disorders: cause or effect? Biochim Biophys Acta. 2010 Jun-Jul;1797(6-7):1130-7.
Parikh, S., et al. A Modern Approach to the Treatment of Mitochondrial Disease. Current Treatment Options in Neurology. 2009 Nov;11(6):414-30.
Parikh, S. The neurologic manifestations of mitochondrial disease. Dev Disabil Res Rev. 2010;16(2):120-8.
Pastural, E., et al. Novel plasma phospholipid biomarkers of autism: mitochondrial dysfunction as a putative causative mechanism. Prostaglandins Leukot Essent Fatty Acids. 2009 Oct;81(4):253-64.
Power, R.A., et al. Carnitine revisited: potential use as adjunctive treatment in diabetes. Diabetologia. 2007 Apr;50(4):824-32.
Rector, R.S., et al. Mitochondrial dysfunction precedes insulin resistance and hepatic steatosis and contributes to the natural history of non-alcoholic fatty liver disease in an obese rodent model. J Hepatol. 2010 May;52(5):727-36.
Schmidt, Charles W. Mito-Conundrum: Unraveling Environmental Effects on Mitochondria. Environmental Health Perspectives. 2010 July; 118(7).
Scirocco, A., et al. Exposure of Toll-like receptors 4 to bacterial lipopolysaccharide (LPS) impairs human colonic smooth muscle cell function. J Cell Physiol. 2010 May;223(2):442-50.
Shen, W., et al. Protective effects of R-alpha-lipoic acid and acetyl-L-carnitine in MIN6 and isolated rat islet cells chronically exposed to oleic acid. J Cell Biochem. 2008 Jul 1;104(4):1232-43.
Shekhawat, P.S., et al. Spontaneous development of intestinal and colonic atrophy and inflammation in the carnitine-deficient jvs (OCTN2(-/-)) mice. Mol Genet Metab. 2007 Dec;92(4):315-24.
Shoffner, J., et al. Fever Plus Mitochondrial Disease Could Be Risk Factors for Autistic Regression. J Child Neurol. 2010 Apr;25(4):429-34.
Shokolenko, I., et al. Oxidative stress induces degradation of mitochondrial DNA. Nucleic Acids Res. 2009 May; 37(8): 2539–2548.
Sifroni, K.G., et al. Mitochondrial respiratory chain in the colonic mucosal of patients with ulcerative colitis. Mol Cell Biochem. 2010 Sep;342(1-2):111-5.
Spindler, M., et al. Coenzyme Q10 effects in neurodegenerative disease. Neuropsychiatr Dis Treat. 2009;5:597-610.
Sreekumar, R., et al. Skeletal muscle mitochondrial dysfunction & diabetes. Indian J Med Res. 2007 Mar;125(3):399-410.
Taurines, R., et al. Expression analyses of the mitochondrial complex I 75-kDa subunit in early onset schizophrenia and autism spectrum disorder: increased levels as a potential biomarker for early onset schizophrenia. Eur Child Adolesc Psychiatry. 2010 May;19(5):441-8.
Weissman, J.R., et al. Mitochondrial Disease in Autism Spectrum Disorder Patients: A Cohort Analysis. PLoS One. 2008;3(11):e3815.
Zhang, H., et al. Combined R–alpha-lipoic acid and acetyl-L-carnitine exerts efficient preventative effects in a cellular model of Parkinson’s disease. J Cell Mol Med. 2010 Jan;14(1-2):215-25.