Kelly Dorfman, MS, LND writes about nutritional interventions for children with mitochondrial dysfunction and autism.
Mitochondrial dysfunction and autism often go hand in hand. William is a six year old with an autism diagnosis. He made encouraging initial gains with extensive intervention until his progress hit a plateau.
A developmental specialist reassessed him noting that his muscle tone and stamina were unusually low. She recommended a metabolic specialist to rule out mitochondrial dysfunction.
What Are Mitochondria?
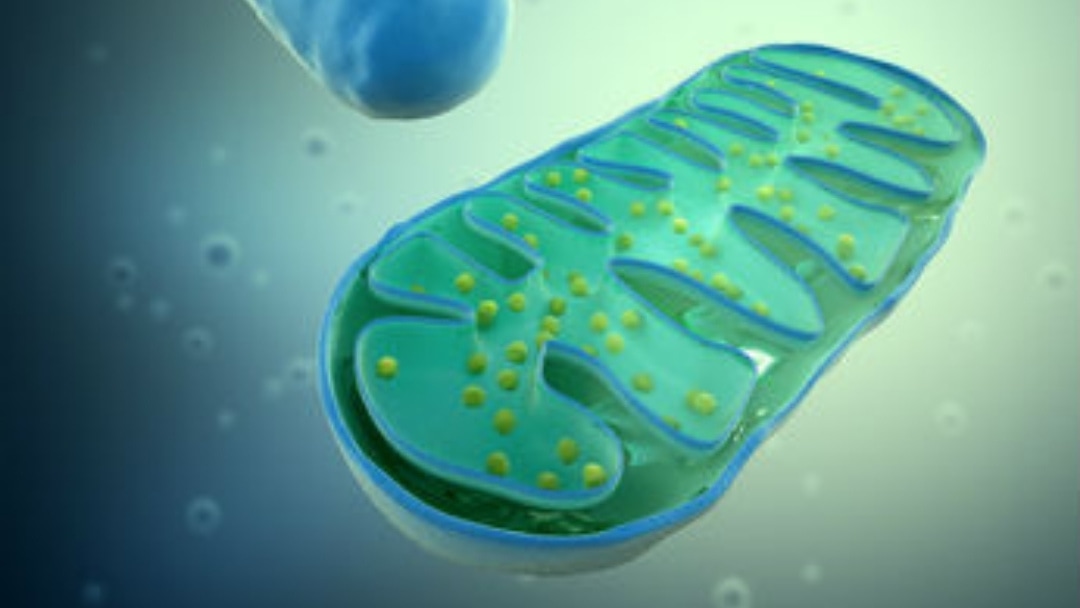
Each cell contains tiny organelles called mitochondria. The job of the mitochondria is to provide the chemical energy the cell and body needs to operate. The cell cannot use sugar or fats directly. Partially broken down fats and carbohydrates must be converted into adenosine triphosphate (ATP), the cell’s main source of energy.
What Is Mitochondrial Dysfucntion?
Children with significant low tone may have mitochondrial dysfunction. Aggressive antibiotic use, heavy metals and pesticides can all injure the mitochondria. The DNA of the mitochondria is separate from and more fragile than the DNA found in the nucleus of the cell.
Common environmental toxins can damage the DNA of the mitochondria altering the cell’s future ability to produce energy. The result is loss of muscle tone and stamina. In mitochondrial dysfunction, muscle tone is low so youngsters need to search for ways to stabilize soft muscles. They may be restless because a comfortable resting position cannot be found. Teachers may complain of poor attention span when in reality the child is chronically distracted by body discomfort.
In rare cases, a child may have one of a limited number of identified mitochondrial defects. The known disorders can only be diagnosed by muscle biopsy and are characterized by serious symptoms (such as an inability to walk). A vast majority of those with low tone suffer from inefficiency, not disease.
Because a partial diagnosis does not exist, a painful biopsy is unlikely to provide useful information except in extreme cases.
Disease Versus Dysfunction
Some mitochondria are more efficient than others because of the influence of different environmental and genetic factors. Well-functioning mitochondria create readily available and sustained energy resulting in toned and well-formed muscles. When these muscles are exercised, they get stronger steadily and predictably.
Whether a child has a known mitochondrial disorder or dysfunction, the only treatment is nutritional. Many nutrients are critical for mitochondrial function but there is a basic cocktail that addresses the most important components.
The Mitochondria Cocktail
Vitamin B-1 and/or B-2
Thiamine (vitamin B-1) and riboflavin (vitamin B-2) are both required co-factors for different parts of energy making. The last step of energy making involves converting ADP (adenosine diphosphate) to ATP.
This step happens down a chain of five protein complexes named Complex I, II, III, IV and V, respectively. Complex I requires vitamin B-1 to stimulate its enzymes. Both Complex I and II require vitamin B-2.
Some children do well with thiamine but get irritated with riboflavin and vice versa. In other cases, both B-vitamins plus B-3 (as niacinamide) are necessary.
Because it is hard to know what to support (without a specific diagnosis), the B-vitamins should be added one at a time. The problem area can be pinpointed by observing the response to intervention. Some children will have a clear response to one B-vitamin or may need them all.
A typical mitochondria formula may contain 50-100mg each of vitamins B-1, B-2 and/or B-3. Keep in close contact with the supervising medical professional and adjust the B-vitamins if the child becomes agitated.
Vitamin E (Mixed Tocopherols)
The mitochondria must be protected against damage from destructive molecules called free radicals. These volatile substances are a normal by-product of metabolism but a healthy body has the capacity to clean them up. When too many get into the mitochondria, they damage the membrane and disrupt energy production.
Vitamin E is an important anti-free radical agent for protecting and healing these membranes. The dose range used is 100-400IU.
Vitamin E is well tolerated, and it has no known toxicity. Natural vitamin E is usually derived from wheat or soy. In rare cases, this may cause allergic problems.
Acetyl-L-Carnitine (ALC)
Carnitine is a simple protein made up of the amino acids methionine and lysine. Research suggests that carnitine helps maintain the membranes of the mitochondria. In addition, ALC helps facilitate the transport and utilization of fats so they can be used to make energy.
For mitochondrial disorders, ALC or the prescription version, Carnitor, is dosed at 50 to 100 mg per kg of body weight. It can sometimes cause irritability or stomach distress but is not toxic.
Bottom Line
The mitochondria can be more efficient if they are fed properly. Healthy mitochondria provide the sustained energy necessary for optimal growth and development.
About Kelly Dorfman MS LND
Kelly Dorfman is one of the world’s foremost experts on using nutrition therapeutically to improve brain function, energy and mood. Kelly’s special talent for integrating information from many sources and finding practical solutions has made her a popular speaker and workshop leader. She lectures extensively and is a member of Platform (formerly the National Speakers Association) and has been featured on numerous television programs including CNN’s American Morning.
Kelly’s award winning book, Cure Your Child With Food: The Hidden Connection Between Nutrition and Childhood Ailments (formerly known as What’s Eating Your Child) was given rave reviews by Publishers Weekly and the Washington Post.

As a go-to expert on nutrition issues, Kelly is frequently interviewed and quoted in the media. She has been featured in articles in The Wall Street Journal, Parade, Bethesda magazine, Living Without magazine, and the Huffington Post.
Kelly holds a master’s degree in nutrition/biology and is a licensed nutrition dietitian. She is a co-founder of Developmental Delay Resources, which has merged with Epidemic Answers. You can find out more about Kelly and her practice at kellydorfman.com
Still Looking for Answers?
Visit the Epidemic Answers Practitioner Directory to find a practitioner near you.
Join us inside our online membership community for parents, Healing Together, where you’ll find even more healing resources, expert guidance, and a community to support you every step of your child’s healing journey.
Sources & References
Andreazza, A.C., et al. Mitochondrial complex I activity and oxidative damage to mitochondrial proteins in the prefrontal cortex of patients with bipolar disorder. Arch Gen Psychiatry. 2010 Apr;67(4):360-8.
Balcells, Cristy. Autism & Mitochondrial Disorders: How Much Do We Really Know?. MitoAction.org. 29 Jan 2009
Beal, M.F., et al. Therapeutic approaches to mitochondrial dysfunction in Parkinson’s disease. Parkinsonism Relat Disord. 2009 Dec;15 Suppl 3:S189-94.
Bradford, B.L., et al. Mitochondrial Dysfunction and Type 2 Diabetes. Science. 2005 Jan 21;307(5708):384-7.
Bradstreet, J.J., et al. Biomarker-guided interventions of clinically relevant conditions associated with autism spectrum disorders and attention deficit hyperactivity disorder. Altern Med Rev. 2010 Apr;15(1):15-32.
Burchell, V.S., et al. Targeting mitochondrial dysfunction in neurodegenerative disease: Part I. Expert Opin Ther Targets. 2010 Apr;14(4):369-85.
Burchell, V.S., et al. Targeting mitochondrial dysfunction in neurodegenerative disease: Part II. Expert Opin Ther Targets. 2010 May;14(5):497-511.
Davi, Alyssa. Has Your Child with Autistic Symptoms Been Properly Screened for a Subset of Mitochondrial Disease Known as OXPHOS?…Probably Not. Autism File. 2010; 36.
Dehley, Leanna M., et al. The Effect of Mitochondrial Supplements on Mitochondrial Activity in Children with Autism Spectrum Disorder. J Clin Med. 2017 Feb; 6(2): 18.
Ferrer, et al. Early involvement of the cerebral cortex in Parkinson’s disease: convergence of multiple metabolic defects. Prog Neurobiol. 2009 Jun;88(2):89-103.
Filipek, P.A., et al. Relative carnitine deficiency in autism. J Autism Dev Disord. 2004 Dec;34(6):615-23.
Haas, R.H., et al. Mitochondrial disease: a practical approach for primary care physicians. Pediatrics. 2007 Dec;120(6):1326-33.
Hao, J., et al. Mitochondrial nutrients improve immune dysfunction in the type 2 diabetic Goto-Kakizaki rats. J Cell Mol Med. 2009 Apr;13(4):701-11.
Herbert, M.R. Contributions of the environment and environmentally vulnerable physiology to autism spectrum disorders. Curr Opin Neurol. 2010 Apr;23(2):103-10
James, S.J., et al. Cellular and mitochondrial glutathione redox imbalance in lymphoblastoid cells derived from children with autism. FASEB J. 2009 Aug;23(8):2374-83.
Kato, T. The role of mitochondrial dysfunction in bipolar disorder. Drug News Perspect. 2006 Dec;19(10):597-602.
Kelley, R.I. Evaluation and Treatment of Patients with Autism and Mitochondrial Disease. Kennedy Krieger Institute, Division of Metabolism.
Klehm, M., et al. Clinician’s Guide to the Management of Mitochondrial Disease: A Manual for Primary Care Providers. MitiAction.org. 2014.
Konradi, C., et al. Molecular evidence for mitochondrial dysfunction in bipolar disorder. Arch Gen Psychiatry. 2004 Mar;61(3):300-8.
Korson, M. Mitochondrial Disease and Patient Challenges. MitoAction. 2008.
Leib, S., et al. Mitochondrial Oxidative Phosphorylation (OXPHOS) Dysfunction: A Newly Emerging Category of Autistic Spectrum Disorder Information for Primary Care Physicians. MitoAction.org. 2010.
Liu, J. The effects and mechanisms of mitochondrial nutrient alpha-lipoic acid on improving age-associated mitochondrial and cognitive dysfunction: an overview. Neurochem Res. 2008 Jan;33(1):194-203.
Long, J., et al. Mitochondrial decay in the of old rats: ameliorating effect of alpha-lipoic acid and acetyl-L-carnitine. Neurochem Res. 2009 Apr;34(4):755-63.
Mabalirajan, U., et al. Effects of vitamin E on mitochondrial and asthma features in an experimental allergic murine model. J Appl Physiol. 2009 Oct;107(4):1285-92.
Maes, M., et al. Coenzyme Q10 deficiency in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is related to fatigue, autonomic and neurocognitive symptoms and is another risk factor explaining the early mortality in ME/CFS due to cardiovascular disorder. Neuro Endocrinol Lett. 2009;30(4):470-6.
Maes, M., et al. Lower plasma Coenzyme Q10 in depression: a marker for treatment resistance and chronic fatigue in depression and a risk factor to cardiovascular disorder in that illness. Neuro Endocrinol Lett. 2009;30(4):462-9.
Morino, K., et al. Molecular mechanisms of insulin resistance in humans and their potential links with mitochondrial dysfunction. Diabetes. 2006 Dec;55 Suppl 2:S9-S15.
Noland, R.C., et al. Carnitine insufficiency caused by aging and overnutrition compromises mitochondrial performance and metabolic control. J Biol Chem. 2009 Aug 21;284(34):22840-52.
Oliveira, G., et al. Mitochondrial dysfunction in autism spectrum disorders: a population-based study. Dev Med Child Neurol. 2005 Mar;47(3):185-9.
Palmieri, L., et al. Mitochondrial dysfunction in autism spectrum disorders: cause or effect? Biochim Biophys Acta. 2010 Jun-Jul;1797(6-7):1130-7.
Parikh, S., et al. A Modern Approach to the Treatment of Mitochondrial Disease. Current Treatment Options in Neurology. 2009 Nov;11(6):414-30.
Parikh, S. The neurologic manifestations of mitochondrial disease. Dev Disabil Res Rev. 2010;16(2):120-8.
Pastural, E., et al. Novel plasma phospholipid biomarkers of autism: mitochondrial dysfunction as a putative causative mechanism. Prostaglandins Leukot Essent Fatty Acids. 2009 Oct;81(4):253-64.
Power, R.A., et al. Carnitine revisited: potential use as adjunctive treatment in diabetes. Diabetologia. 2007 Apr;50(4):824-32.
Rector, R.S., et al. Mitochondrial dysfunction precedes insulin resistance and hepatic steatosis and contributes to the natural history of non-alcoholic fatty liver disease in an obese rodent model. J Hepatol. 2010 May;52(5):727-36.
Schmidt, Charles W. Mito-Conundrum: Unraveling Environmental Effects on Mitochondria. Environmental Health Perspectives. 2010 July; 118(7).
Scirocco, A., et al. Exposure of Toll-like receptors 4 to bacterial lipopolysaccharide (LPS) impairs human colonic smooth muscle cell function. J Cell Physiol. 2010 May;223(2):442-50.
Shen, W., et al. Protective effects of R-alpha-lipoic acid and acetyl-L-carnitine in MIN6 and isolated rat islet cells chronically exposed to oleic acid. J Cell Biochem. 2008 Jul 1;104(4):1232-43.
Shekhawat, P.S., et al. Spontaneous development of intestinal and colonic atrophy and inflammation in the carnitine-deficient jvs (OCTN2(-/-)) mice. Mol Genet Metab. 2007 Dec;92(4):315-24.
Shoffner, J., et al. Fever Plus Mitochondrial Disease Could Be Risk Factors for Autistic Regression. J Child Neurol. 2010 Apr;25(4):429-34.
Shokolenko, I., et al. Oxidative stress induces degradation of mitochondrial DNA. Nucleic Acids Res. 2009 May; 37(8): 2539–2548.
Sifroni, K.G., et al. Mitochondrial respiratory chain in the colonic mucosal of patients with ulcerative colitis. Mol Cell Biochem. 2010 Sep;342(1-2):111-5.
Spindler, M., et al. Coenzyme Q10 effects in neurodegenerative disease. Neuropsychiatr Dis Treat. 2009;5:597-610.
Sreekumar, R., et al. Skeletal muscle mitochondrial dysfunction & diabetes. Indian J Med Res. 2007 Mar;125(3):399-410.
Taurines, R., et al. Expression analyses of the mitochondrial complex I 75-kDa subunit in early onset schizophrenia and autism spectrum disorder: increased levels as a potential biomarker for early onset schizophrenia. Eur Child Adolesc Psychiatry. 2010 May;19(5):441-8.
Weissman, J.R., et al. Mitochondrial Disease in Autism Spectrum Disorder Patients: A Cohort Analysis. PLoS One. 2008;3(11):e3815.
Zhang, H., et al. Combined R–alpha-lipoic acid and acetyl-L-carnitine exerts efficient preventative effects in a cellular model of Parkinson’s disease. J Cell Mol Med. 2010 Jan;14(1-2):215-25.