When babies are born, their immune systems are immature and require time for development and for immune function to improve. As they come in contact with environmental stimuli such as microbes, food particles, and other antigens, their immune systems learn how to differentiate “friend” from “foe”. They also learn how to effectively eliminate harmful substances (pathogens, toxins, etc.) from the body.
Problems arise when a baby’s immune system is not allowed to develop naturally.
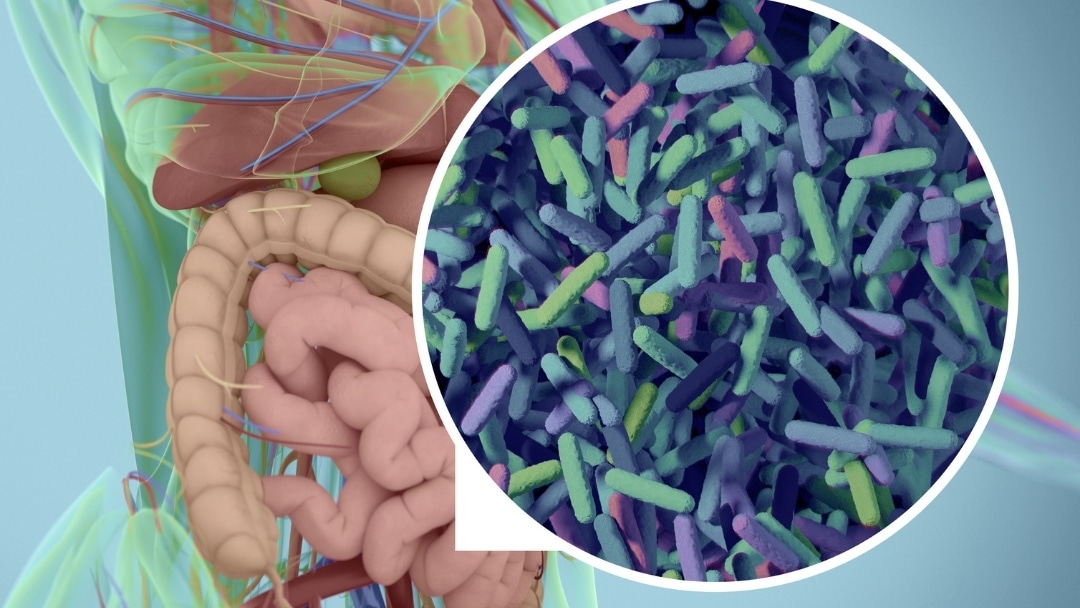
The Gastrointestinal Tract
The headquarters of the immune system is the gastrointestinal tract. Since approximately 90% of known pathogens enter the body through the gastrointestinal tract, it makes sense that the vast majority of the immune system would be located here.
Within the first few months of an infant’s life, the gastrointestinal tract goes from being completely sterile (in the womb) to becoming colonized by hundreds, perhaps even thousands, of different types of microorganisms. These colonies of microorganisms are critical to immune system development and to fundamental biological processes such as digestion, nutrient assimilation, as well as detoxification.
The microorganisms in the gastrointestinal tract play a critical role in immune function. Good germs in the gut are known to provide essential “building blocks” for the human immune system, especially with regard to regulatory functions (the parts that keep the immune system “in check”). A lack of these essential building blocks can result in an immune system that cannot shut itself off, and can treat benign substances as “invaders”.
Relatively recently, scientists have discovered that disruptions to the development of the critical colonies of microbiota (microorganisms) in the gut can lead to a variety of immune system dysfunctions.
The Function of Germs in Immune Function
“Germ-free” animal models where animals are raised with sterile guts, have demonstrated that absence of good bacteria in their guts results in defective gut-associated lymphoid tissue (GALT), the tissue of the intestines that is considered the headquarters of immune function in our bodies. In other words, animals raised without gut bacteria develop immune systems that do not work properly, and thus the animals become very sick.
If you compare the number of human cells versus bacterial cells that each of us contains, we are more bacterial than we are human. Of all the cells in our body, we are about 10% human and 90% bacterial. If you compare the number of human genes in our body compared to bacterial genes, we are 1% human and 99% bacterial. All of these bacteria that we carry around weigh an average of 2 to 5 lbs. Other microorganisms that can inhabit the gut include yeasts, parasites, viruses, and protozoans.
The primary roles of “healthy” intestinal microorganisms include metabolism, defense, and immunomodulation (regulation of the immune system). The metabolic functions of good germs include (but are not limited to) vitamin synthesis, fermentation of carbohydrates, and energy production. Good germs are also necessary to protect the gastrointestinal tract from pathogenic invaders by producing bacteriocidins (highly specific “antibiotics”) and by competing with pathogenic organisms for food and space.
Still Looking for Answers?
Visit the Epidemic Answers Practitioner Directory to find a practitioner near you.
Join us inside our online membership community for parents, Healing Together, where you’ll find even more healing resources, expert guidance, and a community to support you every step of your child’s healing journey.
Sources & References
Aguilera, M., et al. Antibiotic-induced dysbiosis alters host-bacterial interactions and leads to colonic sensory and motor changes in mice. Gut Microbes. 2015;6(1):10-23.
Atladóttir, H.Ó., et al. Autism after infection, febrile episodes, and antibiotic use during pregnancy: an exploratory study. Pediatrics. 2012 Dec;130(6):e1447-54.
Bora, S.A., et al. Regulation of vitamin D metabolism following disruption of the microbiota using broad spectrum antibiotics. J Nutr Biochem. 2018 Jun;56:65-73.
Borchers, A.T., et al. Probiotics and immunity. Journal of Gastroenterology. 44 (2009): 26-46.
Microbial-host molecular exchange and its functional consequences in early mammalian life. Science. 2020 May 8;368(6491):604-607.
Hamad, A.F., et al. Prenatal antibiotics exposure and the risk of autism spectrum disorders: A population-based cohort study. PLoS One. 2019 Aug 29;14(8):e0221921.
Hanaway, P. Balance of Flora, GALT, and Mucosal Integrity. Alternative Therapies in Health and Medicine. Sep-Oct 2006;12(5):52-60; quiz 61-2.
Hrncir,T., et al. Gut microbiota and lipopolysaccharide content of the diet influence development of regulatory T cells: studies in germ-free mice. BMC Immunology. 9 (2008): 65.
Hyman, M.A. Is the Cure for Brain Disorders Outside the Brain? Alternative Therapies in Health and Medicine. Nov-Dec 2007;13(6):10-5.
Kang, D.W., et al. Microbiota Transfer Therapy alters gut ecosystem and improves gastrointestinal and autism symptoms: an open-label study. Microbiome. 2017 Jan 23;5(1):10.
Kitano, H., et al. Robustness trade-offs and host-microbial symbiosis in the immune system. Molecular Systems Biology. 2 (2006).
Korpela, K., et al. Maternal Fecal Microbiota Transplantation in Cesarean-Born Infants Rapidly Restores Normal Gut Microbial Development: A Proof-of-Concept Study. Cell, 2020.
Liu, Z., et al. Tight junctions, leaky intestines, and pediatric diseases. Acta Paediatricia. 94 (2005): 386-393.
Mine, Y., et al. Surfactants Enhance the Tight-Junction Permeability of Food Allergens in Human Intestinal Epithelial Caco-2 Cells. International Archives of Allergy and Immunology. 2003 Feb;130(2):135-42.
Montalto, M., et al. Fecal Calprotectin Concentrations in Patients with Small Intestinal Bacterial Overgrowth. Digestive Diseases. 2008;26(2):183-6.
Moser, L.A. Astrovirus Increases Epithelial Barrier Permeability Independently of Viral Replication. Journal of Virology. 2007 Nov;81(21):11937-45.
Nankova, B.B. Nicotinic Induction of Preproenkephalin and Tyrosine Hydroxylase Gene Expression in Butyrate-Differentiated Rat PC12 Cells: A Model for Adaptation to Gut-Derived Environmental Signals. Pediatric Research. 2003 Jan;53(1):113-8.
O’Hara, A.M., et al. The gut flora as a forgotten organ. European Molecular Biology Organization Report 7, no 7 (July 2006): 688-693.
Rautava, S., et al. The Development of Gut Immune Responses and Gut Microbiota: Effects of Probiotics in Prevention and Treatment of Allergic Disease. Current Issues in Intestinal Microbiology. 2002 Mar;3(1):15-22.
Savino, F., et al. Lactobacillus reuteri (American Type Culture Collection Strain 55730) versus simethicone in the treatment of infantile colic: a prospective randomized study. Pediatrics. 2007 Jan;119(1):e124-30.
Strauch, U.G., et al. Influence of intestinal bacteria on induction of regulatory T cells: lessons from a transfer model of colitis. Gut 54 (2005):1546-1552.
Tobacman, J.K. Review of Harmful Gastrointestinal Effects of Carrageenan in Animal Experiments. Environmental Health Perspectives. 2001 Oct;109(10):983-94.
Vael, C., et al. Early intestinal Bacteroides fragilis colonization and development of asthma. BMC Pulmonary Medicine. 2008 Sep 26;8:19.
Warner, B.B. The contribution of the gut microbiome to neurodevelopment and neuropsychiatric disorders. Pediatr Res. 2019 Jan;85(2):216-224.
Wexler, H. Bacteroides: the Good, the Bad, and the Nitty-Gritty. Clinical Microbiology Reviews 20, no. 4 (October 2007): 593-621.
White, E., et al. The Effect of Nutritional Therapy for Yeast Infection (Candidiasis) in Cases of Chronic Fatigue Syndrome. Journal of Orthomolecular Medicine. 2005;20(3).
Resources
Books
Galland, Leo. The Effect of Intestinal Microbes on Systemic Immunity. Excerpted from Power Healing. Random House, 1998.
Kellman, Raphael. The Microbiome Diet: The Scientifically Proven Way to Restore Your Gut Health and Achieve Permanent Weight Loss. Da Capo Lifelong Books, 2015.
Sachs, Jessica Snyder. Good Germs, Bad Germs: Health and Survival in a Bacterial World. Hill and Wang, 2007.