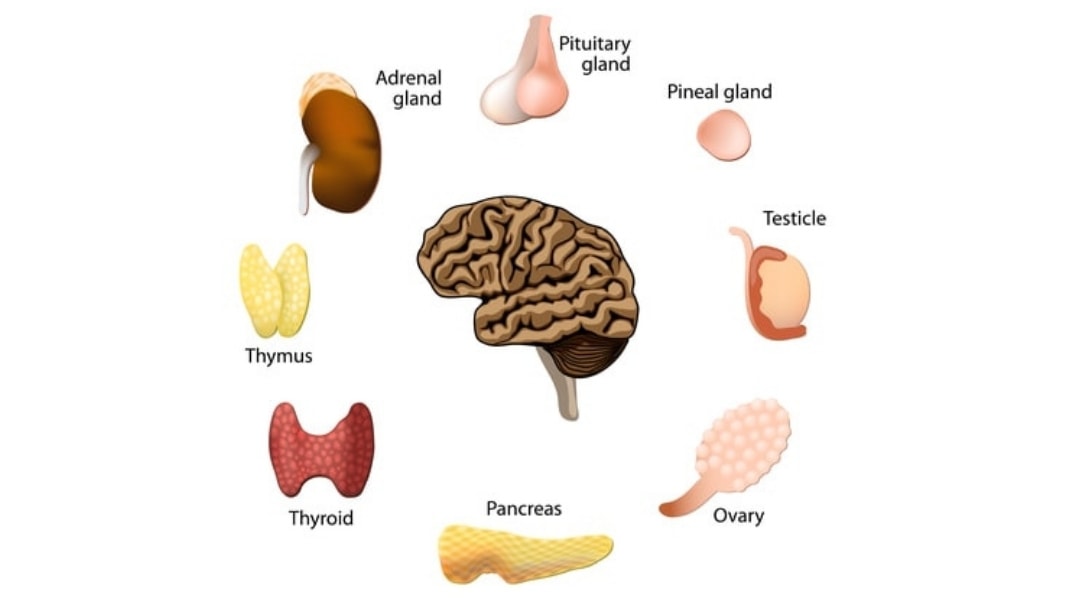
The thyroid gland is a butterfly-shaped gland that has two lobes situated on either side of the windpipe (trachea). It is located in the front of the neck just below the Adam’s apple (larynx). This little gland produces hormones that regulate the body’s:
- Metabolism
- Heart
- Digestive function
- Temperature
- Reproduction
- Growth
- Weight
- Cognitive ability
- Mood
- Muscle control
- Brain development
- Bone maintenance
- Toxicity, especially radiation
In order for the thyroid gland to produce adequate amounts of hormones, the diet must include enough iodine, which is a trace mineral, that can be found in the following foods:
- Dried seaweed
- Codfish
- Turkey breast
- Navy beans
- Tuna
- Eggs
- Baked potato
- Strawberries
- Cranberries
- Bananas
- Dried prunes
- Lobster
- Green beans
- Shrimp
Thyroid Hormones
There are two hormones produced by the thyroid gland that are commonly tested by doctors:
- Triiodothyronine (T3), the more active hormone
- Thyroxine (T4), the more inactive hormone
The thyroid gland produces 20% of the body’s T3 and the other 80% comes from T4 which is converted from the liver or kidneys. The thyroid gland also produces calcitonin from specific cells called C-cells. Calcitonin is a rather unique hormone that works to control calcium and potassium by regulating blood calcium and phosphate levels in the body. The releasing of these hormones from this gland is controlled by:
- Thyrotrophin-Releasing Hormone (TRH), which comes from the hypothalamus in the brain
- Thyroid Stimulating Hormone (TSH), which comes from the pituitary gland
These two hormones form a feedback loop called the Hypothalamic-Pituitary-Thyroid Axis. When stress increases and becomes chronic, this causes cortisol levels to elevate continuously and the Hypothalamic-Pituitary-Thyroid Axis becomes dysfunctional. When this happens, the thyroid produces much lower levels of thyroid hormone leading to “hypothyroidism”. When too much thyroid hormone is produced it leads to “hyperthyroidism”.
Hypothyroidism and Neurodevelopmental Disorders
According to Raphael Kellman MD, hypothyroidism or low thyroid has become very common among mothers of children who were later diagnosed with autism, learning disabilities, ADHD and developmental delays. Dr. Kellman is a New York internist specializing in autism spectrum disorders who believes that many children with autism have inherited their mother’s thyroid dysfunction called Congenital Hypothyroidism. See this story on Micah and Congenital Hypothyroidism and autism.
The following symptoms of hypothyroidism (low thyroid) in children are very similar to symptoms of autism:
- Speech delays
- Developmental delays
- Cognitive dysfunction
- Hyperactivity
- Lethargy
- Hypotonia (low muscle tone)
- Fine motor delays
- Attention deficit disorders
- Repetitive motions
- Social deficits
- Communication deficits
- Fear
- Anxiety
- Depression
- Gastrointestinal issues
- Constipation
- Feeding and eating problems
Iodine Deficiency Check
If you are unsure whether your child is iodine deficient or not, put a small amount of liquid iodine (nickel or quarter size) on the inside of the wrist and watch how long it take the body to absorb the iodine into the skin. If the skin absorbs the iodine right away then your child is iodine deficient. If the iodine takes 24 hours or so to absorb, then your child has sufficient amount of iodine.
Still Looking for Answers?
Visit the Epidemic Answers Practitioner Directory to find a practitioner near you.
Join us inside our online membership community for parents, Healing Together, where you’ll find even more healing resources, expert guidance, and a community to support you every step of your child’s healing journey.
Sources & References
Adams, J.B., et al. Mercury in first-cut baby hair of children with autism versus typically-developing children. Toxicological & Environmental Chemistry. 2007 Jun;70(12):1046-51.
Adams, J.B., et al. Mercury, Lead, and Zinc in Baby Teeth of Children with Autism Versus Controls. Journal of Toxicology and Environmental Health. 2007 Jun;70(12):1046-51.
Alampi, J.D., et al. Gestational Exposure to Toxicants and Autistic Behaviors using Bayesian Quantile Regression. Am J Epedemiol. 2021 Sep 1;190(9):1803-1813.
Mixtures of persistent organic pollutants are found in vital organs of late gestation human fetuses. Chemosphere. 2021 Nov;283:131125.
Braun, J.M., et al. Gestational exposure to endocrine-disrupting chemicals and reciprocal social, repetitive, and stereotypic behaviors in 4- and 5-year-old children: the HOME study. Environ Health Perspect. 2014 May;122(5):513-20.
Cohen, Patricia. Roundup Maker to Pay $10 Billion to Settle Cancer Suits. The New York Times. 24 Jun 2020.
Geier, M.R., et al. The potential importance of steroids in the treatment of autistic spectrum disorders and other disorders involving mercury toxicity. Med Hypotheses. 2005;64(5):946-54.
Gunatilake, S., et al. Glyphosate’s Synergistic Toxicity in Combination with Other Factors as a Cause of Chronic Kidney Disease of Unknown Origin. Int J Environ Res Public Health. 2019 Jul 31;16(15):2734.
Hansen, J.B., et al. Prenatal exposure to bisphenol A and autistic- and ADHD-related symptoms in children aged 2 and5 years from the Odense Child Cohort. Environ Health. 2021 Mar 12;20(1):24.
Harley, K.G., et al. Changes in Latina Women’s Exposure to Cleaning Chemicals Associated with Switching from Conventional to “Green” Household Cleaning Products: The LUCIR Intervention Study. Environ Health Perspect. 2021 Sep;129(9):97001.
Hauser, P., et al. Resistance to thyroid hormone: implications for neurodevelopmental research on the effects of thyroid hormone disruptors.
Toxicol Ind Health. 1998 Jan-Apr;14(1-2):85-101.
Hertz-Picciotto, I., et al. Polybrominated diphenyl ethers in relation to autism and developmental delay: a case-control study. Environ Health. 2011 Jan 5;10(1):1.
Hinhumpatch, P., et al. Oxidative DNA damage and repair in children exposed to low levels of arsenic in utero and during early childhood: application of salivary and urinary biomarkers. Toxicol Appl Pharmacol. 2013;273(3):569-79.
Holmes, A., et al. Reduced Levels of Mercury in First Baby Haircuts of Autistic Children. International Journal of Toxicology. Jul-Aug 2003;22(4):277-85.
Jafari, M.H., et al. The Relationship Between the Level of Copper, Lead, Mercury and Autism Disorders: A Meta-Analysis. Pediatric Health, Medicine and Therapeutics. 21 Sep 2020(11):369—378.
Jafari, T., et al. The association between mercury levels and autism spectrum disorders: A systematic review and meta-analysis. J Trace Elem Med Biol. 2017 Dec;44:289-297.
Julvez, J., et al. Early life multiple exposures and child cognitive function: A multi-centric birth cohort study in six European countries. Environ Pollut. 2021 Sep 1;284:117404.
Kern, J.K., et al. A biomarker of mercury body-burden correlated with diagnostic domain specific clinical symptoms of autism spectrum disorder. Biometals. 2010;23(6):1043-51.
Konkel, L. Phthalates and Autistic Traits: Exploring the Association between Prenatal Exposures and Child Behavior. Environ Health Perspec. 2020 Oct;128(10):104001.
Landrigan, P.J., et al. Children’s vulnerability to toxic chemicals: a challenge and opportunity to strengthen health and environmental policy. Health Aff. (Millwood). 2011 May;30(5):842-50.
Lombardi, C., et al. Residential proximity to pesticide application as a risk factor for childhood central nervous system tumors. Environ Res. 2021 Jun;197:111078.
Lyall, K., et al. Prenatal Serum Concentrations of Brominated Flame Retardants and Autism Spectrum Disorder and Intellectual Disability in the Early Markers of Autism Study: A Population-Based Case-Control Study in California. Environ Health Perspect. 2017 Aug 30;125(8):087023.
Messer, A. Mini-review: polybrominated diphenyl ether (PBDE) flame retardants as potential autism risk factors. Physiol Behav. 2010 Jun 1;100(3):245-9.
Napoli, E., et al. Toxicity of the flame-retardant BDE-49 on brain mitochondria and neuronal progenitor striatal cells enhanced by a PTEN-deficient background. Toxicol Sci. 2013 Mar;132(1):196-210.
Napolitano, G., et al. Is zinc deficiency a cause of subclinical hypothyroidism in Down syndrome? Ann Genet. 1990;33(1):9-15.
Palmer, R.F., et al. Proximity to point sources of environmental mercury release as a predictor of autism prevalence. Health and Place. 2009 Mar;15(1):18-24.
Peltier, M.R., et al. Maternal Hypothyroidism Increases the Risk of Attention-Deficit Hyperactivity Disorder in the Offspring. Am J Perinat. 2020 Oct 21.
Samsel, A., et al. Glyphosate, pathways to modern diseases II: Celiac sprue and gluten intolerance. Interdiscip Toxicol. 2013 Dec;6(4):159-84.
Samsel, A., et al. Glyphosate, pathways to modern diseases III: Manganese, neurological diseases, and associated pathologies. Surg Neurol Int. 2015 Mar 24;6:45.
Samsel, A, et al. Glyphosate’s suppression of cytochrome P450 enzymes and amino acid biosynthesis by the gut microbiome: Pathways to modern diseases. Entropy. 2013;15:1416–1463.
Venâncio, P., et al. Anti-N-methyl-D-aspartate receptor encephalitis with positive serum antithyroid antibodies, IgM antibodies against mycoplasma pneumoniae and human herpesvirus 7 PCR in the CSF. Pediatr Infect Dis J. 2014 Aug;33(8):882-3.
Wang, H.L., et al. Case-Control Study of Blood Lead Levels and Attention Deficit Hyperactivity Disorder in Chinese Children. Environmental Health Perspectives. 2008 Oct;116(10):1401-6.
Watt, T., et al. Is Thyroid Autoimmunity per se a Determinant of Quality of Life in Patients with Autoimmune Hypothyroidism? Eur Thyroid J. 2012;1(3):186-92.
Wong, S., et al. Autism, Mitochondria and Polybrominated Diphenyl Ether Exposure. CNS Neurol Disord Drug Targets. 2016;15(5):614-23.
Xu, C.L., et al. Anti-N-methyl-D-aspartate receptor encephalitis with serum anti-thyroid antibodies and IgM antibodies against Epstein-Barr virus viral capsid antigen: a case report and one year follow-up. BMC Neurol. 2011 Nov 29;11:149.
Resources
Articles
The Environmental Working Group. Body Burden: The Pollution in Newborns. 14 Jul 2005.
Swan, Shanna, et al. Reproductive Problems in Both Men and Women Are Rising at an Alarming Rate: A likely culprit is hormone-disrupting chemicals. Scientific American, 16 Mar 2021.
Books
Hong, Maria Rickert. Almost Autism: Recovering Children from Sensory Processing Disorder, A Reference for Parents and Practitioners. 2014.
Markley, Lisa, et al. The Essential Thyroid Cookbook: Over 100 Nourishing Recipes for Thriving with Hypothyroidism and Hashimoto’s. Blue Wheel Press, 2017.
Perro, Michelle, et al. What’s Making Our Children Sick?: How Industrial Food Is Causing an Epidemic of Chronic Illness, and What Parents (and Doctors) Can Do About It. Chelsea Green Publishing, 2017.
Rogers, Sherry. Detoxify or Die. Prestige Publishing, 2002.
Wachter, Kenneth W., et al. Offspring: Human Fertility Behavior in Biodemographic Perspective. National Academy of Sciences, 2003.
Videos
A Global Fertility Crisis – Dr. Shanna Swan