What Are Gastrointestinal Disorders?
Living with gastrointestinal disorders is very painful and distressful for children and heartbreaking for parents, especially when a child has limited language to express how they feel. One thing is certain: the faces of children with gastrointestinal disorders tell the true story. Some of the common pediatric gastrointestinal disorders are:
- Constipation
- Abdominal pain due to gas and bloating
- Diarrhea
- Malabsorption
- Clostrium difficile infection
- Small intestinal bacterial overgrowth (SIBO)
- Enterocolitis
- Failure to thrive
- Helicobacter pylori infection
- Inflammatory bowel disease
- Vomiting
- Gastroesophageal reflux disease (GERD)
- Intestinal pathogens
- Nutritional deficiencies
- Lymphoid hyperplasia
- Colic
- Intestinal permeability
- Intestinal inflammation
- Ulcerative colitis
- Food allergies such as gluten and casein intolerance
- Food selectivity
- Narrow food preferences
- Specific food/texture preferences
Gastrointestinal disorders will inevitably affect the child’s behaviors, mood, sensory, nervous, neurological and immunological systems if left untreated.
For small and/or nonverbal children, suspect a gastrointestinal disorder if you find him or her constantly draped belly down over couch or chair arms. Children do this to relieve the uncomfortable and/or painful pressure in their abdomen. They may not have enough language or experience to tell you about this pain.
What Your Doctor May Tell You About Gastrointestinal Disorders
Most pediatricians will refer their patients to a gastroenterologist if gastrointestinal disorders are suspected. The doctor will initially collect information from doing a general patient intake, physical exam, requesting parental information on the child’s gastrointestinal history, and doing screen tests such as blood, urine and stool, ultrasounds or e-rays.
In difficult cases, further testing may be needed such as:
- Colonoscopy
- EGD (upper endoscopy)
- Pill cam study (which is a tiny camera in a capsule that takes photos of the small intestine)
- Gastrointestinal disorders lower scope
- Biopsy
Medication is the most common form of treatment by a gastrointestinal specialist. Diet is usually not recommended as a contributing factor, unless it is determined that there is a need for dietary intervention such as celiac.
In the case of abdominal pain, doctors will give medication to treat and manage the pain but may not have a long-term solution if your child’s gastrointestinal condition is chronic. If your child has a developmental disorder, the gastrointestinal specialist may tell you that your child’s disorder and behaviors are a separate issue from the gastrointestinal disorder with which your child has been diagnosed.
Another Way to Think About Gastrointestinal Disorders
The Microbiome
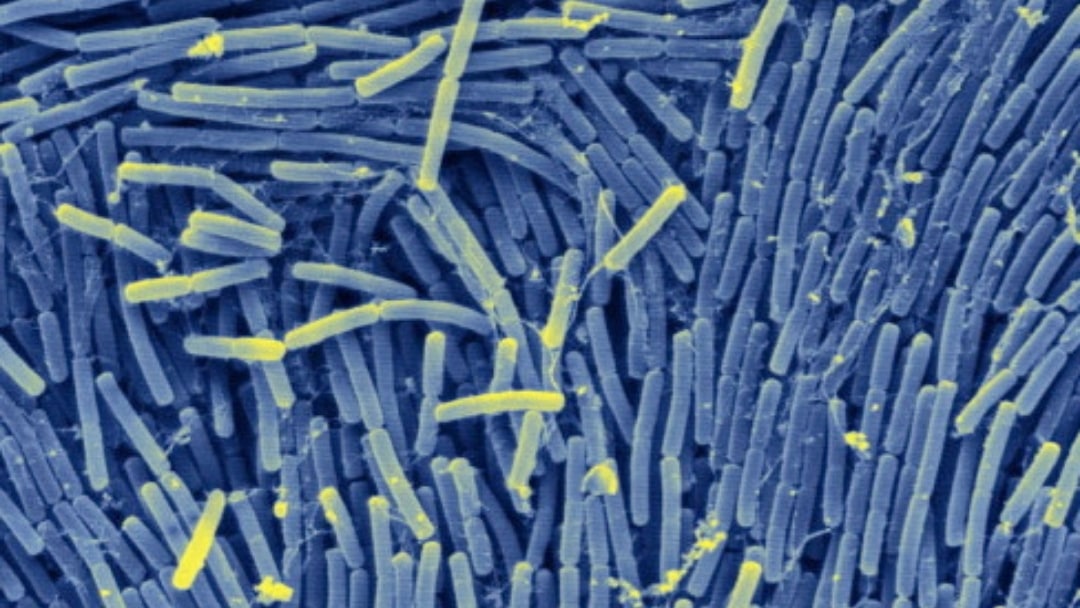
When your child has a gastrointestinal disorder, the first thing we must think of is “microbiome”. The microbiome was discovered in the late 1990s as part of the gastrointestinal system and is home to trillions of bacteria.
The human gut “microbiota” is the name given to the colonies of microbes that live in our digestive system. These gut microbes are vitally important for communication with the brain and the immune system. It is believed that 70% of our immune system is located in the digestive tract.
Canadian researcher Derrick McFabe PhD has demonstrated how changes in the gut bacteria affect brain functioning and behaviors, thus proving the theory of the gut/brain axis. He has shown how specific bad gut bacteria can alter the gut/brain connection as demonstrated in children with autism.
Neurotransmitters
Also in our brain are chemical messengers that transmit signals from one neuron to another telling the brain and body what to do. These messengers are called neurotransmitters, and they are also located in our gastrointestinal tract, which allows for communication with the brain.
If the gastrointestinal tract develops a common condition called leaky gut syndrome, then this means there has been too much foreign matter that has permeated the gut lining. As a result, many bad pathogens, bacteria, viruses, yeast, fungus and parasites can populate the gastrointestinal tract and disrupt communication with the neurotransmitters in the brain causing the neurotransmitters to misfire.
This process begins the development of an autoimmune disorder, and, if this happens, your child may experience many problems such as:
- Developmental delays
- Muscle tone issues
- Mood swings
- Aggression
- Sensory overload
- Sympathetic dominance of the nervous system (fight or flight)
Therefore, no matter what gastrointestinal disorder your child may have, begin with healing the microbiome.
Gastrointestinal Disorders Healing Checklist
Use homeopathy specific for gastrointestinal disorders:
- Nux vomica
- Carbo vegetalis
- Lycopodium
- China officinalis
- Argentum nitricum
Consider using Schueller’s cell tissue salts, which can be effective as well. Sequential homeopathy can also be specific for gastrointestinal symptoms if needed.
Still Looking for Answers?
Visit the Epidemic Answers Practitioner Directory to find a practitioner near you.
Join us inside our online membership community for parents, Healing Together, where you’ll find even more healing resources, expert guidance, and a community to support you every step of your child’s healing journey.
Sources & References
Aguilera, M., Cerda-Cuellar, M., Martinez, V. Antibiotic-induced dysbiosis alters host-bacterial interactions and leads to colonic sensory and motor changes in mice. Gut Microbes. 2015;6(1):10-23.
Aroniadis, O.C., Brandt, L.J. Fecal microbiota transplantation: past, present and future. Curr Opin Gastroenterol. 2013;29(1):79-84.
Assa, A., Vong, L., Pinnell, L.J., Avitzur, N., Johnson-Henry, K.C., Sherman, P.M. Vitamin D deficiency promotes epithelial barrier dysfunction and intestinal inflammation. J Infect Dis. 2014;210(8):1296-305.
Buccigrossi, V., Nicastro, E., Guarino, A. Functions of intestinal microflora in children. Curr Opin Gastroenterol. 2013;29(1):31-8.
Carding, S., Verbeke, K., Vipond, D.T., Corfe, B.M., Owen, L.J. Dysbiosis of the gut microbiota in disease. Microb Ecol Health Dis. 2015;26:26191.
Cucchiara, S., Stronati, L., Aloi, M. Interactions between intestinal microbiota and innate immune system in pediatric inflammatory bowel disease. J Clin Gastroenterol. 2012;46 Suppl:S64-6.
Fukuda, K., Fujita, Y. Determination of the discriminant score of intestinal microbiota as a biomarker of disease activity in patients with ulcerative colitis. BMC Gastroenterol. 2014;14:49.
Galland, L. The gut microbiome and the brain. J Med Food 2014; 17(12): 1261-72.
Guandalini, S. Are probiotics or prebiotics useful in pediatric irritable bowel syndrome or inflammatory bowel disease? Front Med (Lausanne). 2014;1:23.
Guandalini, S., Cernat, E., Moscoso, D. Prebiotics and probiotics in irritable bowel syndrome and inflammatory bowel disease in children. Benef Microbes. 2015;6(2):209-17.
Jakobsen, C., Paerregaard, A., Munkholm, P., Wewer, V. Environmental factors and risk of developing paediatric inflammatory bowel disease — a population based study. 2007-2009. J Crohns Colitis. 2013;7(1):79-88.
Manichanh, C., Borruel, N., Casellas, F., Guarner, F. The gut microbiota in IBD. Nat Rev Gastroenterol Hepatol. 2012;9(10):599-608.
Savino, F., et al. Lactobacillus reuteri (American Type Culture Collection Strain 55730) versus simethicone in the treatment of infantile colic: a prospective randomized study. Pediatrics. 2007 Jan;119(1):e124-30.
Scirocco, A., et al. Exposure of Toll-like receptors 4 to bacterial lipopolysaccharide (LPS) impairs human colonic smooth muscle cell function. J Cell Physiol. 2010 May;223(2):442-50.
Sela, D.A., Mills, D.A. The marriage of nutrigenomics with the microbiome: the case of infant associated bifidobacteria and milk. Am J Clin Nutr. 2014;99(3):697S-703S.
Shekhawat, P.S., et al. Spontaneous development of intestinal and colonic atrophy and inflammation in the carnitine-deficient jvs (OCTN2(-/-)) mice. Mol Genet Metab. 2007 Dec;92(4):315-24.
Sifroni, K.G., et al. Mitochondrial respiratory chain in the colonic mucosal of patients with ulcerative colitis. Mol Cell Biochem. 2010 Sep;342(1-2):111-5.
West, C.E., Renz, H., Jenmalm, M.C., Kozyrskyj, A.L., Allen, K.J., Vuillermin, P., et al. The gut microbiota and inflammatory noncommunicable diseases: associations and potentials for gut microbiota therapies. J Allergy Clin Immunol. 2015;135(1):3-13; quiz 4.
Resources
Books
Campbell-McBride, Natasha. Gut and Psychology Syndrome: Natural Treatment for Autism, Dyspraxia, A.D.D., Dyslexia, A.D.H.D., Depression, Schizophrenia. 2010
Chutkin, Robin. The Microbiome Solution: A Radical New Way to Heal Your Body from the Inside Out. Avery, 2016